Pages in this section:
20th Meeting of the European Association for the Study of Diabetes Eye Complications Study Group (EASDec)
Paris, France 21st - 22nd May 2010
FREE PAPER SESSIONS
- A 25-YEAR FOLLOW-UP STUDY OF TYPE 1 DIABETIC PATIENTS: NEPHROPATHY AT FOLLOW-UP IS ASSOCIATED WITH PROLIFERATIVE RETINOPATHY AT BASELINE
- J. Grauslund1, C. Karlberg1, C. Falk1, A. Green2, A.K. Sjølie1
- 1Department of Ophthalmology, Odense University Hospital, Odense - Denmark
- 2Center for National Clinical Databases, South, Odense University Hospital, Odense - Denmark
-
- INTRODUCTION. Is proliferative retinopathy an indicator of long-term incident nephropathy in type 1 diabetes?
- PURPOSE. To examine proliferative retinopathy as a marker of incident nephropathy in a 25-year follow-up study of a population-based cohort of Danish type 1 diabetic patients.
- METHODS. All type 1 diabetic patients from Fyn County, Denmark, were identified as of July 1 1973. 184 patients were examined in both 1981-82 and 2007-08. The level of retinopathy was graded by ophthalmoscopy at baseline and nine-field colour fundus photos at follow-up. A single spot urine was used to evaluate nephropathy at both examinations.
- RESULTS. Proliferative retinopathy was present in 29 patients (15.8%) at baseline. At follow-up, these patients were more likely to macroalbuminuria (20.7% vs. 6.5%) than patients without proliferative retinopathy at baseline. In a multivariate logistic regression adjusted for baseline age, sex, duration of diabetes, smoking, HbA1, systolic and diastolic blood pressure, odds ratio of nephropathy (micro- and macroalbuminuria combined) was 2.98 (95% confidence interval 1.18-7.51, p=0.02) for patients with proliferative retinopathy at baseline as compared to those without. At follow-up there was a close relationship between retinopathy and nephropathy. The level of macroalbuminuria was 4.3%, 4.6% and 13.0% for patients with no or mild non-proliferative retinopathy, moderate non-proliferative retinopathy and proliferative retinopathy, respectively.
- CONCLUSIONS. Proliferative retinopathy is an independent marker of long-term nephropathy in type 1 diabetes. This suggests a causal link and should be investigated in upcoming studies.
-
- DIABETES AS A RISK FACTOR FOR POST-CRVO NEOVASCULARISATION
- M. Paques1, E. Champion1, N. Sedira2, J.F. Girmens1, J.A. Sahel1, E. Héron2, S. Feldman2
- 1Clinical Investigation Center 503 of the Quinze-Vingts Hospital – Paris
- 2Internal medicine and diabetes, Quinze-Vingts Hospital - Paris
- INTRODUCTION. Neovascularisation is the most feared complication of CRVO. Here we performed a systematic analysis of clinical risk factors for post-CRVO neovascularisation.
- PURPOSE. To investigate clinical factors related to the occurrence of neovascularisation in a cohort of patients with CRVO.
- METHODS. Retrospective study of 63 patients with CRVO examined in a single centre. The presence or absence of neovascularisation was correlated with demographic factors, medical history and metabolic parameters (body mass index, waist circumference and HbA1c).
- RESULTS. Among the 63 patients with CRVO (aged 63 ± 12 years), 22 showed neovascularisation (35%). The 16 diabetic patients had a higher incidence of neovascularisation than the 47 non-diabetics (56 vs. 28%, p = 0.039). The risk factors showed a different profile depending on the presence or absence of diabetes. In patients without diabetes, age was associated with risk of neovascularisation (43% of ≥ 65 had neovascular vs 15% younger, p = 0.038) but not HbA1c, arterial pressure or gender. Instead, in diabetics HbA1c (p = 0.004) and waist circumference (p = 0.045) were correlated with the risk of neovascularisation, regardless of the existence of diabetic retinopathy.
- CONCLUSIONS. Diabetes, with or without retinopathy is the major risk factor of post-CRVO neovascularisation. The risk is correlated to HbA1c levels. The severity of CRVO in diabetics shows that even in the absence of clinically detectable retinopathy, the resilience of the retinal vasculature to stress is impaired.
-
- THE SIGNIFICANCE OF MICROANEURYSMS AND HAEMORRHAGES WITHIN ONE OPTIC DISC DIAMETER OF THE FOVEA
- H. M. Wharton1, P. M. Dodson1,2, J. M. Gibson2
- 1Diabetes & Endocrinology Unit, Heartlands Hospital, Birmingham – United Kingdom
- 2Ophthalmology Department, Heartlands Hospital, Birmingham – United Kingdom
-
- INTRODUCTION. Microaneurysms and haemorrhages within the macula area are a poor predictor of macular oedema as shown by optical coherence tomography (OCT). Our research suggests that it is safe and cost effective to screen patients who present with these surrogate markers annually.
- PURPOSE. To determine whether microaneurysms (ma) and haemorrhages (hm) within one optic disc diameter of the fovea (ma/hm<1DD) are significant predictors of macular oedema.
- METHODS. Data were collected over a one-year period from patients attending digital diabetic retinopathy screening. Patients who presented with ma/hm<1DD also had an OCT scan. The fast macula scan on the Stratus OCT was used and an ophthalmologist reviewed the scans to determine whether macular oedema was present. Macular oedema was identified by thickening on the OCT cross-sections. Patients were split into two groups. Group one (325 eyes) included those with best VA6/9 and group two (30 eyes) with best VA ≤6/12. Only patients who had no other referable features of diabetic retinopathy were selected.
- RESULTS. In group one, 6 (1.8%) out of 325 eyes showed thickening on the OCT and were referred to hospital eye service (HES) for further investigation. In group two, 6 (20%) out of 30 eyes showed thickening and were referred to HES.
- CONCLUSIONS. Ma/hm<1DD become more significant predictors of macular oedema when VA is reduced. Results confirm the grading criteria concerning microaneurysms predicting macular oedema for referable maculopathy in the English national screening programme. OCT is a useful method to accurately identify patients requiring referral to HES.
-
- LASER TREATMENT OF DIABETIC MACULAR OEDEMA: TOWARD A LESS INVASIVE APPROACH
- S Vujosevic1, E Pilotto2, E Bottega2, E Midena1,2
- 1Fondazione G.B. Bietti, IRCCS, Roma – Italy
- 2Department of Ophthalmology, University of Padova, Padova - Italy
-
- INTRODUCTION. Visible end point argon laser photocoagulation is associated with photoreceptor destruction and decrease in retinal sensitivity in patients with diabetic macular oedema (DME).
- PURPOSE. To evaluate and compare microperimetry and fundus autofluorescence (FAF) after subthreshold micropulse diode laser (MPDL) vs modified ETDRS photocoagulation for DME.
- METHODS. A prospective, randomised trial of 62 eyes (50 patients) with untreated DME was performed. All patients underwent: best corrected visual acuity determination(BCVA), slit lamp biomicroscopy, FAF, OCT, microperimetry and fluorescein angiography (FA), before and after treatment. BCVA, OCT, microperimetry, FAF were repeated at 1, 3, 6, 9 and 12 months follow-up. FA was repeated at 6 and 12 months.
- RESULTS. Before treatment, the two treatment groups were similar. At 12 months: BCVA remained stable in both groups (p>0.05); mean central retina thickness (CRT) decreased in both groups (p<0.05); mean central 4° and 12° retina sensitivity (RS) increased in the MPDL group (p=0.02, p=0.0075), and decreased in the ETDRS group (p=0.2, p=0.0026). There was no significant difference in both BCVA and CRT between the two treatment groups (p=0.48, p=0.29), whereas there was significant difference in 4° and 12° RS (p=0.04 and p<0.0001). FAF never changed in MPDL group. In the ETDRS group, FAF increased up to 9 months, and decreased in 6 eyes (20%) at 12 months.
- CONCLUSIONS. MPDL improves retinal sensitivity and does not change FAF, although it is equally effective when measured by BCVA and OCT, as modified ETDRS laser photocoagulation in DME. These data encourage the use of new less aggressive laser approach in the treatment of DME.
-
- SAFETY PROFILES OF RANIBIZUMAB IN DIABETIC VERSUS NON-DIABETIC AMD PATIENTS FROM RANDOMISED CONTROLLED TRIALS
- F. Bandello1, G. Burian2, A. Weichselberger2, Y. Hashad2
- 1Department of Ophthalmology, University Vita-Salute Scientific Institute San, Raffaele, Via Olgettina, 60, 20132 Milano – Italy
- 2Novartis Pharma AG, Basel - Switzerland
-
- INTRODUCTION. The safety profile of ranibizumab in AMD patients with an underlying diabetic condition may differ from that known from the general AMD patient population. Safety profiles are compared between diabetic (Db) and non-diabetic (nDb) AMD patients in randomised controlled trials (RCT).
- PURPOSE. To identify potential diabetes-related safety signals in AMD patients treated with monthly ranibizumab in RCTs.
- METHODS. A meta-analysis was performed using pooled 1-year incidences of potential risks of ranibizumab in DbAMD (n=523) and nDbAMD (n=3213) patients treated monthly with 0.5mg ranibizumab in ANCHOR, MARINA, PIER, SAILOR, EXCITE, and EXTEND I studies. Safety risks comprised ocular/non-ocular adverse events (AEs) and serious AEs (SAEs). Multiple occurrences of the same event in a patient were counted once.
- RESULTS. The two patient groups were similar in baseline demographics and ocular characteristics. Mean duration of diabetes in DbAMD group was 8.9 years. Overall, there was no evidence of increased risk of ocular/non-ocular AEs and SAEs in DbAMD compared to nDbAMD patients. Numerical differences were observed for cardiac disorders (AEs/SAEs: 9.6/6.7% DbAMD, 6.8/3.2% nDbAMD), infections and infestations (AEs/SAEs: 26.6/4.4% DbAMD, 22.8/2.7% nDbAMD), and metabolism and nutrition disorders (AEs/SAEs:13.0/1.5% DbAMD, 6.4/0.3% nDbAMD). The observed incidences of the AEs/SAEs in DbAMD group can be attributed to the underlying diabetic condition.
- CONCLUSIONS. The safety profiles of diabetic and non-diabetic patients from the AMD trials show signals consistent with the epidemiology of diabetes; no increased ocular or non-ocular safety risks of ranibizumab treated DbAMD patients were noted.
-
- EVALUATION OF A NEW RANIBIZUMAB RE-TREATMENT CRITERIA BASED ON THE RESOLVE STUDY
- P. Massin1, Y. Hashad2, G. Burian2, A. Weichselberger2
- 1Assistance Publique des Hôpitaux de Paris, Ophthalmology Department, Hopital Lariboisiere, Universite Paris VII, 2 rue Ambroise Pare, 75010 - Paris
- 2Cedex 10, France Novartis Pharma AG, Basel - Switzerland
-
- INTRODUCTION. Flexible re-treatment criteria help to individualise treatment of DME patients. Here, we evaluate a new re-treatment concept based on treatment responses of RESOLVE patients to ranibizumab
- PURPOSE. To evaluate a new ranibizumab re-treatment concept based on dose interruption/re-initiation upon disease-stability/disease-activity in DME patients.
- METHODS. 12-month randomised controlled trial; patients randomised 1:1:1 to ranibizumab 0.3 to 0.6 mg (51) or 0.5 to 1.0 mg (51) or sham (49) with 3-monthly injections and re-treatment based on disease-stability/disease-activity criteria. Disease-stable when VA, or VA+CRT changes between the minimum and maximum values over three last visits (including current) were within margins of 3 letters/50μm. Effectiveness of re-treatment criteria assessed based on VA and CRT response.
- RESULTS. Disease-stability criteria fulfilled in 84% based on VA (74% based on VA+CRT); mean (±SE) change in VA/CRT 1M after treatment upon detecting disease-stability was +1.1±0.7 letters (n=72)/-2.8±4.1µm (n=69) based on VA (+0.1±0.6 letters (n=60)/-8.0±4.0µm (n=58) based on VA+CRT) indicating no clinically significant improvement upon re-treatment on diseases-stability. Disease-activity: 50 re-initiation injections between M3-M11, 42% (n=21) and 64% (n=32) fulfilled VA, and VA and/or CRT criteria; mean (±SE) change in VA/CRT 1M after treatment re-initiation was +10.0±1.3 letters (n=20)/-133±25.9µm (n=20) based on VA (+6.0±1.38 letters (n=31)/-123.8±17.3µm (n=31) based on VA and/or CRT), suggesting a clinically relevant VA/CRT improvement upon re-treatment on disease-activity.
- CONCLUSIONS. This evaluation suggests that ranibizumab treatment interruption/re-initiation based on disease-stability/disease-activity criteria derived from monthly VA and CRT assessments is a viable concept to provide guidance for individualised treatment in DME.
-
- VISUAL ACUITY RESPONSE TO RANIBIZUMAB STRATIFIED BY BASELINE CHARACTERISTICS IN DIABETIC MACULAR OEDEMA (DME) (RESOLVE STUDY)
- L.L. Hansen
- University Hospital Freiburg, Killianstr.5, 79106 Freiburg - Germany
- INTRODUCTION. The treatment effect of ranibizumab on visual acuity may depend on the patients' demographic or disease characteristics in the RESOLVE study.
- PURPOSE. Identify subgroups of DME-patients who responded differentially to ranibizumab treatment.
- METHODS. 12-month, multicenter, double-masked randomised controlled trial; 151 patients randomised to 0.3 to 0.6 mg ranibizumab (n=51), 0.5 to 1.0 mg ranibizumab (n=51), or sham (n=49). Three initial monthly injections, followed by re-treatment based on success/futility/safety criteria (laser as rescue). Treatment-response assessed by mean change in BCVA (letters) from baseline to Month 12 and stratified by baseline demographics/disease characteristics.
- RESULTS. At Month 12, mean BCVA (letters) change from baseline was 10.3 for ranibizumab (pooled groups) vs –1.4 for sham (p<0.0001). Mean BCVA change from baseline to Month 12 by characteristic for pooled ranibizumab group vs sham: CRT: 7.8 vs –3.2 (≤400µm), 7.8 vs 1.6 (>400µm); DME-type: 9.2 vs 1.9 (focal), 6.4 vs –2.1 (diffuse); diabetes-type: 14.1 vs 0.1 (Type I), 7.6 vs –0.1 (Type II); BCVA (letters): 8.6 vs –1.0 (≤60), 7.1 vs 0.6 (>60); diabetes-duration: 7.4 vs 2.7 (<10yrs), 8.0 vs –1.2 (≥10yrs); DME-duration: 8.6 vs –1.2 (≤3mo), 5.8 vs 1.1 (>3–≤12mo), 10.1 vs 0.0 (>12mo); BP (systolic/diastolic mmHg): 8.3 vs 1.1 (≥140/90), 6.7 vs –2.5 (<140/90).
- CONCLUSIONS. Ranibizumab consistently improved BCVA in all subgroups compared with sham, largest numerical differences for patients with thin retina, diabetes Type I, and long history of diabetes. Further studies are required to confirm findings.
-
- EVALUATION OF AN INTRAVITREOUS DEXAMETHASONE DRUG DELIVERY SYSTEM IN PATIENTS WITH PERSISTENT DIABETIC MACULAR OEDEMA
- P.Massin1, G.A. Williams2, J.A. Haller3, B.D. Kuppermann4,M.S. Blumenkranz5, D.V. Weinberg6,C. Chou7, S.M. Whitcup8
- 1Dept. of Ophthalmology, Hôpital Lariboisière, Paris - France
- 2Beaumont Eye Institute, Royal Oak, MI, USA
- 3Wills Eye Institute, Philadelphia, PA, USA
- 4University of California, Irvine, Irvine, CA, USA
- 5Stanford University, Stanford, CA, USA
- 6Medical College of Wisconsin, Milwaukee, WI, USA
- 7Eisai Medical Research, Inc., Ridgefield Park, NJ, USA
- 8Allergan, Inc., Irvine, CA, USA
-
- PURPOSE. To evaluate the safety and efficacy of dexamethasone in an intravitreous drug delivery system (DDS) in patients with persistent diabetic macular oedema (DME).
- METHODS. Eyes with DME ≥ 90 days' duration were randomised to observation or treatment with 350 μg or 700 μg dexamethasone DDS.
- RESULTS. At day 90, a ≥ 10-letter BCVA improvement occurred in 33.3% of patients in the 700-µg dexamethasone DDS group and 12.3% in the observation group (P = .007). Improvements were also seen in macular thickness and fluorescein leakage.
- CONCLUSIONS. Patients with persistent DME respond favourably to treatment with 700 µg dexamethasone DDS. Treatment with an intravitreal sustained-release dexamethasone posterior-segment drug-delivery system produced statistically and clinically significant improvements in visual acuity, macular thickness, and fluorescein leakage in patients with persistent diabetic macular oedema
-
- CORRELATIONS BETWEEN VASCULAR RESPONSE TO FLICKER LIGHT AND RETINAL FUNCTION IN NORMOTENSIVE PATIENTS WITH DIABETES WITHOUT DIABETIC RETINOPATHY
- A. Lecleire-Collet1, A. Erginay1, T. Meas4, M. Paques2, E. Vicaut3, P.J. Guillausseau4, P. Massin1
- 1Department of Ophthalmology, Hôpital Lariboisière, Paris 7 University, Paris – France
- 2Center for Clinical Investigation 503 INSERM, Centre Hospitalier National d'Ophtalmologie des XV-XX, Pierre et Marie Curie-Paris 6 University, Paris - France
- 3Clinical Research Unit, Hôpital Fernand Widal, Paris 7 University, Paris – France
- 4Department of Internal Medicine B, Hôpital Lariboisière, Paris 7 University, Paris - France
-
- INTRODUCTION. The early retinal events preceding the onset of diabetic retinopathy (DR) still remain completely unknown.
- PURPOSE. To assess retinal function and vascular response to flicker light using Dynamic Vessel Analyzer (DVA) in normotensive patients with diabetes without DR, and the correlations between them.
- METHODS. Twenty-eight normotensive patients with diabetes and without DR (11 with type 1, 17 type 2 diabetes) and sex and age-matched control subjects underwent colour vision and contrast sensitivity testing, pattern, full field and multifocal electroretinogram (ERG), and evaluation of the vascular response to flicker light with the DVA.
- RESULTS. In the group of patients with diabetes, cone, rod and inner retinal function as well as the vascular response to flicker light were significantly altered. Among all the subjects included, significant correlations were found between the flicker light-induced vascular response and pattern ERG responses (P 50 amplitude (r = 0.3206), N 95 amplitude (r = -0.2690) and N 95 implicit time (r = -0.3530), rod ERG responses (b-wave implicit time (r = -0.3630), and the sum of amplitudes of the oscillatory potentials (r = 0.3991, and r = 0.3754).
- CONCLUSIONS. In patients with diabetes, neural and vascular dysfunction are both early events and precede the onset of clinically detectable retinopathy. Significant correlations were found between the flicker light-induced vascular response and ERG responses, suggesting that the impairment of the vascular response to flicker light is correlated with neural impairment. Then, the impaired flicker-induced vascular response may not only be explained by the presence of endothelial dysfunction, but also by the neural impairment.
-
-
NEURONAL RETINAL DAMAGE IN NON PROLIFERATIVE DIABETIC RETINOPATHY: AN IN VIVO QUANTITATIVE STUDY
- E. Midena1,2, F. Martini1, A. Rediu1, M. Casciano1, S. Vujosevic2
- 1Department of Ophthalmology, University of Padova, Padova – Italy
- 2Fondazione G.B. Bietti, IRCCS, Roma - Italy
-
- INTRODUCTION. A controversy still exists about the retinal neuronal damage in early diabetic retinopathy (DR).
- PURPOSE. To investigate this issue at a microscopic level, in humans, in vivo and with a non-invasive technique.
- METHODS. Ninety-eight subjects were enrolled: 68 diabetics with untreated DR and 30 normals. Twenty patients had no DR (no DR group), 22 had non-proliferative DR without macular oedema (no ME group),and 26 had macular oedema (ME group). Proliferative retinopathy was an exclusion criterion. Full ophthalmic examination, stereoscopic fundus photos, and spectral domain-OCT (SD-OCT:RS-3000, Nidek, Japan) were performed. After automatic segmentation of retinal layers, mean thickness of each layer was calculated in the foveal and pericentral area. All measurements were performed twice by two independent graders.
- RESULTS. In the groups no DR and no ME mean thickness of each inner retinal layer was significantly reduced compared to controls (p<.001), both in fovea and pericentral area. No significant difference was found for outer retinal layers(p=.10). In DME eyes, the thickness of all retinal layers was significantly increased (p<.001) compared to all other groups. Micro- and macro-cystic spaces contributed to increased thickness, without interference with automatic layering. The inter-grader agreement was at least substantial.
- CONCLUSIONS. Thinning of the neural retina in diabetics without retinopathy and with non-proliferative DR without ME is confirmed in vivo, in a non-invasive way. Retinal thinning is due to a selective thinning of inner retinal layers, suggesting an early neurodegenerative process. Automatic intraretinal layering by SD-OCT may be a useful tool to diagnose and monitor early intraretinal changes in DR.
-
- RETINAL OXYGENATION IN PATIENTS WITH DIABETIC RETINOPATHY
- E. Stefánsson, S.H. Hardarson, O.B. Olafsdottir
- University of Iceland/Landspítali-University Hospital, Department of Ophthalmology, Reykjavik - Iceland
-
- INTRODUCTION. Diabetic retinopathy (DR) is believed to involve hypoxia. However, measurements of human retinal oxygenation are scarce.
- PURPOSE. The purpose of the study was to measure retinal vessel oxygen saturation in patients with diabetic retinopathy.
- METHODS. The retinal oximeter (Oxymap ehf., Reykjavik, Iceland) is composed of a fundus camera, beam splitter, light filters and specialised software. One first or second degree temporal arteriole and venule were measured in one eye of 31 healthy subjects and 28 patients with diabetic retinopathy. The diabetic patients had background DR (BDR, n=6), macular oedema (DME, n=7), pre-proliferative or proliferative DR (pre-PDR/PDR, n=7) or proliferative DR and a history of successful treatment (treated PDR, n=8). Statistical analysis was performed with one-way ANOVA and Dunnett's post test.
- RESULTS. Retinal arteriolar oxygen saturation was 93±4% (mean±SD) in healthy subjects; 103±6% in BDR; 102±6% DME; 100±5% in pre-PDR/PDR; and 100±9% in treated PDR. The corresponding saturation in retinal venules was 58±6% (healthy), 70±4% (BDR), 66±9% (DME), 67±8% (pre-PDR/PDR) and 66±11% (treated PDR). Both arteriolar and venular saturation were higher in each group of DR patient than in healthy subjects (p<0.05).
- CONCLUSIONS. Possible explanations for higher retinal vessel saturation in diabetic patients include shunting of blood from arterioles to venules, increased total retinal blood flow, degeneration of tissue and decreased diffusion of oxygen through thicker vessel walls.
-
- TNF-α IN DIABETIC RETINOPATHY
- C. Gustavsson, C.D. Agardh, E. Agardh
- Department of Clinical Sciences, Malmö, Skåne University Hospital, Lund University - Sweden
-
- INTRODUCTION. The cytokine TNF-α is possibly involved in the pathogenesis and a potential target for treatment of diabetic retinopathy (DR).
- PURPOSE. To study the association of TNF-α and DR in humans, rats, and mice.
- METHODS. TNF-α was assessed in serum from diabetic subjects with proliferative DR (PDR) compared to those with no or non-proliferative DR (no/NPDR), in serum and vitreous from diabetic subjects with PDR, and in aqueous humor and serum from diabetic subjects with no/NPDR compared to non-diabetic subjects. TNF-α mRNA-expression was assessed in ischemic diabetic and non-diabetic rat retina, and its influence on the expression of the endothelial dysfunction marker VCAM-1 in diabetic TNF-α knockout mice.
- RESULTS. TNF-α levels were higher in serum from PDR compared to no/NPDR subjects (p<0.001) and in diabetic compared to non-diabetic subjects (p<0.001). The vitreous/serum ratio was high in both diabetic PDR subjects (2:1) and in non-diabetic subjects with other vitreoretinal diseases (3.4:1). TNF-α levels in aqueous humor did not differ. TNF-α mRNA expression was higher in ischemic compared to non-ischemic rat retina (p≤0.012) and VCAM-1 expression was higher in TNF-α deficient than in wild-type mouse retina (p<0.001), regardless of diabetes.
- CONCLUSIONS. TNF-α in serum seems to be a marker for both diabetes and DR severity, but the vitreous results suggests that it is involved in several retinal disorders, supported by ischemia-induced but not diabetes-induced TNF-α expression in rats. However, TNF-α also seems to be essential for basal endothelial regulation. The complexity of TNF-α as treatment target has to be further clarified.
-
- PERICYTE-ENDOTHELIAL CELL INTERACTIONS IN CO-CULTURE MODELS MIMICKING THE DIABETIC RETINAL MICROENVIRONMENT
-
E. Beltramo, S. Tarallo, E. Berrone, M. Porta
- Department of Internal Medicine, University of Turin, Italy
-
- INTRODUCTION. Pericytes regulate vascular tone and perfusion pressure in capillaries, and endothelial cell proliferation (EC). Thiamine (T) and benfotiamine (BT) are able to counteract high glucose-induced damage in vascular cells. We standardised two pericyte (HRP)/EC co-culture models, to mimic the physiological and diabetic retinal microenvironment.
- PURPOSE. Our aim was to evaluate the interactions between co-cultured HRP/EC in terms of proliferation/apoptosis and the possible protective role of T/BT against high glucose-induced damage.
- METHODS. EC and HRP were co-cultured for 8 days in physiological glucose (NG), stable high glucose (HG) and intermittent HG (HGint), with/without T/BT. No-contact model: EC were plated on a membrane suspended into the medium and HRP on the bottom of the same well; cell-to-cell contact model: EC and HRP were plated on the opposite sides of the same membrane. Proliferation (cell counts and DNA synthesis) and apoptosis were measured.
- RESULTS. In the no-contact model, HG reduced proliferation of co-cultured EC/HRP (p=0.001 vs NG) and EC alone (p<0.05) and increased co-cultured EC/HRP apoptosis (p<0.05). In the contact model, both HG and intHG reduced co-cultured EC/HRP proliferation (p<0.05) and increased apoptosis (p<0.05). Stable HG had no effects on HRP in separate cultures. Both EC and HRP proliferated more in co-culture (p<0.05 vs single culture). T/BT countered HG induced-damage in all cases.
- CONCLUSIONS. HRP may be sensitive to soluble factors released by EC cultured in HG concentrations. T and BT counteract this damage. The nature of the soluble factors remains to be clarified.
-
- POSSIBLE POSITIVE EFFECTS OF INSULIN IN EARLY PERICYTE LOSS
-
E. Berrone, E. Beltramo, S. Tarallo, M. Porta
- Department of Internal Medicine, University of Turin - Italy
-
- INTRODUCTION. A pro-survival effect of insulin on microvascular cells has been suggested recently. However, no data are available on the response and expression of glucose transporters in human retinal pericytes (HRP) after insulin stimulation.
- PURPOSE. To verify the effects of insulin on survival, intracellular glucose and expression of glucose transporters (GLUT 1, 2, 3, 4) in HRP cultured in intermittent high glucose (HGint).
- METHODS. Pericytes were kept alternatively in high (HG) or normal (NG) glucose at 48h intervals for 8 days, with or without 100nM or 1µM insulin (Ins). Control cells were cultured in stable NG or HG. GLUT transporter mRNA expression was determined by RT-PCR, intracellular glucose and apoptosis by ELISA and cell proliferation by cell counts.
- RESULTS. HRP express GLUT 1, 3 e 4, but not GLUT2. GLUT1 was increased in HGint (p<0.05 vs NG) and reduced by insulin, when added to HGint (p<0.05 vs HGint). In contrast, GLUT4 was reduced in HGint (p<0.05 vsNG) and increased in the presence of insulin 100nM (p<0.004 vsHGint). GLUT3 mRNA was unchanged in all experimental conditions. In HGint, intracellular glucose levels were increased (p<0.05 vs NG), and reduced by 1µM insulin (p<0.05 vs HGint). Cell counts were reduced in HGint (p<0.05 vs NG) and increased by insulin (p<0.05 vs HGint). Apoptosis increased with HGint (p<0.001 vs NG) and was completely normalised by insulin (p<0.001 vs HGint).
- CONCLUSIONS. Insulin may protect HRP from proliferation damage induced by intermittent HG and influence the expression of glucose transporters.
-
- THE BURDEN OF DIABETIC MACULAR OEDEMA WITH VISUAL IMPAIRMENT
-
P. Lanzetta, M. Gallagher, D. Lakdawalla, K. Van Nuys
- University of Udine, Udine, Italy Novartis Pharma AG, Basel – Switzerland
- Precision Health Economics, Santa Monica, CA – United States of America
-
- INTRODUCTION. Studies of Diabetic Macular Oedema (DME) show a clear and substantial burden associated with the disease. However gaps in the literature necessitate further evidence to understand the global burden of DME, particularly when associated with visual impairment (DME/VI).
- PURPOSE. Quantify and characterise the total societal burden of DME/VI in the US and UK
- METHODS. We compared annual expenditures of patients with DME/VI to those with DM-only using US and UK claims data reflecting real-world utilisations. Descriptive and multivariate tests were performed. Estimates from the literature were used to extrapolate indirect expenditures.
- RESULTS. In 2002-7, annual incident DME/VI cases ranged from 162 to 562 (US) and 10 to 47 (UK). As a proportion of the diabetic population, DME/VI prevalence was 0.14-0.51% (US) and 0.02-0.24% (UK); incidence was 0.08-0.16% (US) and 0.02-0.08% (UK). In 2007, average expenditure per US DME/VI patient was $44,531, compared to $21,990 for DM-only controls, and $35,649 for DME patients without visual impairment. DME/VI expenditures were significantly higher than DM-only expenditures in all but two categories. Indirect costs for DME/VI patients added $13,062, for a total incremental per-patient burden of $35,603 above the DM-only burden, or $4.3 billion in the US alone. A comparison of these results to the UK population will also be presented.
- CONCLUSIONS. DME/VI patients have significantly higher expenditures than DM-only and DME-without-VI controls. As a result, DME and its associated visual impairment contribute billions annually to the global burden of diabetes.
-
- SCREENING FOR DIABETIC RETINOPATHY: A COMPARATIVE TRIAL OF PHOTOGRAPHY AND SCANNING LASER OPHTHALMOSCOPY
- P.J. Wilson1, J.D. Ellis1, C.J. MacEwen1, A. Ellingford2, J. Talbot1, G.P Leese2
- 1Department of Ophthalmology, Ninewells Hospital and Medical School, Dundee – United Kingdom
- 2Department of Diabetes, Ninewells Hospital and Medical School, Dundee – United Kingdom
-
- INTRODUCTION. In many programmes, digital retinal photography has become the primary tool in screening for diabetic retinopathy. Newer technologies such as wide-field scanning laser ophthalmoscopy (WSLO) have been developed, and may offer advantages over existing imaging modalities.
- PURPOSE. To evaluate the sensitivity and specificity of WSLO in the detection of referable diabetic eye disease, and to compare its performance with digital retinal photography.
- METHODS. Patients enrolled into the study underwent non-mydriatic WSLO imaging, then single- and dual-field mydriatic digital retinal photography, and examination with slit lamp biomicroscopy, the reference standard. Grading of retinopathy was performed in a masked fashion.
- RESULTS. A total of 380 patients (759 eyes) were recruited to the study. Technical failure rates for dilated single-field retinal photography, dual-field retinal photography and undilated WSLO were 6.3, 5.8 and 10.8%, respectively (0.005 < p < 0.02 for photography vs. WSLO).
The respective indices for screening sensitivity were 82.9, 82.9 and 83.6% (p > 0.2). Specificity was 92.1, 91.1 and 89.5%, respectively (p > 0.2). - CONCLUSIONS. Sensitivity and specificity for WSLO were similar to retinal photography. The technical failure rate was greater for the WSLO used in this study.
-
- AN EXPERT SYSTEM FOR THE RISK ESTIMATION OF THE PRESENCE OF SIGHT THREATENING DIABETIC RETINOPATHY AND ITS IMPLEMENTATION AS AN INTERNET RESOURCE
- A.N. Stangos1, A.C. Fisher2, A. Eleuteri2, N. Collaer1, D. Broadbent1, S.P. Harding1,3
- 1Clinical Eye Research Centre, St. Paul's Eye Unit, Royal Liverpool University Hospital – United Kingdom
- 2Deprtment of Medical Physics and Clinical Engineering, Royal Liverpool University Hospital - UK
- 3Ophthalmology Research Unit, School of Clinical Sciences, University of Liverpool – United Kingdom
-
- INTRODUCTION. The burden of detection of sight-threatening diabetic retinopathy (STDR) is very large and increasing globally. There is a need to develop new approaches to detecting STDR.
- PURPOSE. To develop an expert system to estimate the risk of STDR from systemic risk factors used in the routine management of people with diabetes (PWD).
- METHODS. Patient records were extracted from a test database developed from 541 patient records extracted from the Liverpool Diabetes Eye Study database. Putative risk factors were assessed for inclusion. Using a generalised linear model (GLM), a graphical web-based implementation was mounted at www.liverpooleye.org (DR_Risk_Expert_System) which is accessible by any internet browser. Area under the receiver operator curve (AUROC) was utilised to measure effectiveness (with 95% CI) of each tested covariate.
- RESULTS. Five putative risk factors (covariates) were identified as significant predictors: duration of disease; diastolic blood pressure (BP); systolic BP; HbA1c; random total cholesterol. Extending the model to a more sophisticated non-linear model based on Gaussian processes did not usefully improve performance. The risk expert system is shown in the figure with example data and output.
-
-
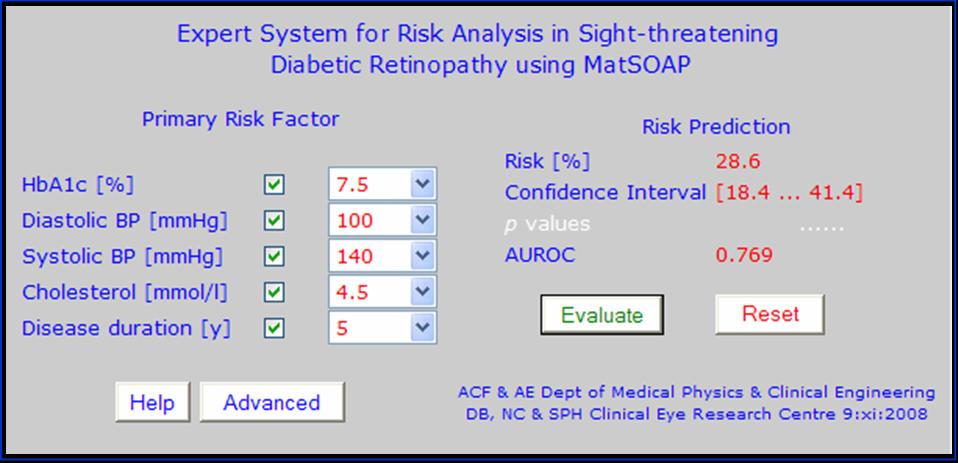
- CONCLUSIONS. An expert system based on non-ophthalmic risk factors can identify PWD at risk of having STDR.
-
-
AUTOMATED “DISEASE/NO DISEASE”
- L. Ribeiro1, H. Palaio2, G. Monteiro2, L. Cristóvão3, J.R. Faria de Abreu1
- 1AIBILI - Association for Innovation and Biomedical Research on Light and Image, Coimbra - Portugal 2Critical Health, Coimbra – Portugal
- 3University Hospital of Coimbra - Portugal
-
- INTRODUCTION. Screening for treatable diabetic retinopathy is crucial. Automated grading will be a major step forward.
- PURPOSE. To assess the performance of automated analysis of retinal photographs for diabetic retinopathy screening.
- METHODS. A set of images from 5,386 patients screened in 2007 were obtained from a non-mydriatic Diabetic Retinopathy Screening Programme of the Central Region of Portugal. Images were graded by an experienced ophthalmologist. To verify if the system misclassifies the referral cases considered urgent, 116 urgent cases registered between 2001 and 2007 were also collected for processing.
The automated grading system (RetmarkerSR) consisted of a software for Microaneuryms (MAs) earmarking, generating two possible outputs: disease / no disease. RetmarkerSR results were compared with the ones manually graded. - RESULTS. The results obtained with RetmarkerSR showed 2,560 patients (48%) as having “no disease” and therefore tagged for next screening and 2,826 patients (52%) as having “disease” and requiring manual grading by an expert. Comparing these results with the grading performed by the ophthalmologist, all eyes considered urgent referrals are included in the “disease” group.
The RetmarkerSR achieved a sensitivity of 96.1% (95% CI (confidence interval) [94.39, 97.89]) with a specificity of 51.7% (95% CI [50.27; 53.07]). From the additional 116 cases collected and considered urgent by the ophthalmologist from 2001 to 2007, the RetmarkerSR only misclassified one case, which was found to be a macular pucker. - CONCLUSIONS. Automated grading of diabetic retinopathy may safely reduce the burden of “disease/no disease” grading in diabetic retinopathy screening programmes.
-
- INTERNET-SERVED EXTERNAL QUALITY ASSURANCE GRADING TESTING IN THE ENGLISH NATIONAL SCREENING PROGRAMME FOR DIABETIC RETINOPATHY
- S.J. Aldington, D.J. Taylor, I.M. Stratton, P.H. Scanlon
- English National Screening Programme for Diabetic Retinopathy, Cheltenham – United Kingdom
-
- INTRODUCTION. Digital retinal screening primarily to detect sight-threatening diabetic retinopathy (STDR) has been implemented by 93 NHS service delivery programmes across England to over 2 million people with diabetes. Over 1500 people (lay graders, optometrists or ophthalmologists) assess retinopathy status and requirement for referral from the images (grading).
- PURPOSE. Provide an internet-served EQA process for local programmes to identify good- and under-performance by individual graders. Provide disease-weighted samples equitably to users and available monthly, so results are clinically relevant, comparable within/between programmes and available in a timely manner.
- METHODS. Monthly tests present users with one of 12 possible ‘blocks' of 30 cases (eyes) comprising two-field 45 degree colour digital retinal images for assessment. Grey-scale, magnification, contrast/brightness tools are available. Users allocate standard Retinopathy (0, 1, 2 or 3) and Maculopathy grade (0 or 1) for each case. User's percentage score shown on completion of monthly test but image review prevented. Local programme administrators analyse more detailed results.
- RESULTS. By January 2010, 1016 users from 90 of the 93 programmes have completed 1 or more monthly tests with overall mean of 78% agreement on R and M grade. Of the 7 blocks so far presented, mean (range) scores are Block 1: 80% (50-97%), 2: 80% (52-100%), 3: 80% (57-97%), 4: 78% (62-92%), 5: 80% (65-90%), 6: 77% (57-88%), 7: 77% (72-85%).
- CONCLUSIONS. Web-served EQA grading tests are an efficient and acceptable method of providing relevant data to screening programmes.
-
- HYPERGLYCEMIA ALTERS RETINAL ENDOTHELIAL CELL GLYCOCALYX: POTENTIAL ROLE OF HEPARANASE 1
- K.I. Wolanska, J.M. Tarr, J.L. Whatmore, R. Chibber
- Peninsula College of Medicine and Dentistry, University of Exeter, Exeter – United Kingdom
-
- INTRODUCTION. Diabetic retinopathy (DR) is thought to be an inflammatory condition associated with increased leukostasis and capillary non-perfusion. Increasing evidence suggests that the endothelial glycocalyx influences the leukocyte-endothelial cell adhesion. Heparanase1 (HPSE) regulates degradation of heparan sulfate (HS) side chains. These form a substantial component of the glycocalyx and can be modified by HPSE in inflammation. Interestingly, Phosphomannopentaose sulfate (PI-88) - a HPSE inhibitor inhibits retinal leukostasis in vivo (Ma et al., 2009).
- PURPOSE. To investigate whether high glucose influences retinal HPSE expression and release leading to altered capillary endothelial cell glycocalyx structure and pericytes function.
- METHODS. Bovine retinal endothelial cells (BREC) and pericytes (BRP) were exposed to normal (NG, 5.6mM), high glucose (HG, 25mM) or mannitol (25mM) for 24h. HPSE expression and secretion were determined by immunoprecipitation and immunoblotting. BREC glycocalyx was labelled with FITC-conjugated wheat germ agglutinin and assessed by a cell based fluorescence assay.
- RESULTS. Glycocalyx was reduced [84±9.6% vs. NG (100%), p<0.001, n = 15] after 24h exposure to HG. HG and mannitol significantly increased HPSE secretion to 185±89% (p<0.001, n=17) and 139±72 (p=0.0048, n=17) vs. NG (100%), respectively after 24h. In BRP HPSE secretion appeared to be markedly reduced after 24h [HG 70±17% vs. NG (100%) p=0.008 n=5].
- CONCLUSIONS. Altered glycocalyx structure and function via glucose-induced HPSE expression may play a role in leukostasis and the pathogenesis of early DR.
-
- PREVALENCE AND TYPES OF DIABETIC RETINOPATHY IN NIGERIA: FINDINGS OF THE NIGERIA NATIONAL BLINDNESS AND VISUAL IMPAIRMENT SURVEY
- F. Kyari1, T. Peto2, S. Sivsubramaniam1, F. Sallo2, G.V.S. Murthy1, C. Gilbert1
- 1International Centre for Eye Health, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT - United Kingdom
- 2Department of Research and Development, Moorfields Eye Hospital NHS Foundation Trust, 162 City Road, London EC1V 2PD – United Kingdom
- INTRODUCTION. Diabetic retinopathy (DR) accounts for 5% of blindness globally but data from West Africa are lacking.
- PURPOSE. To determine the prevalence of DR and describe the types of DR among adults aged >40 years in Nigeria.
- METHODS. A nationally representative sample of 15,027 persons >40 years and older across Nigeria were selected. All (n=13,599) were asked about history of diabetes. 1 in 7 (n=1,722) were examined in detail and had random blood glucose (RBG) testing to construct a normative database. Participants with visual acuity < 6/12 and/or retinopathy seen on undilated fundoscopy had detailed examination and digital retinal photography. Participants with DM were identified from history, RBG of 11.1mmol/l or higher and DR detected on dilated retinal examination and/or images. DR was defined as microaneurysms, dot-blot haemorrhages, new vessels, IRMA; exudates, circinate and CSME at the macula. Images were graded by Moorfields Eye Hospital Reading Centre.
- RESULTS. From the normative data, the prevalence of DM was 3.3%(95%CI 2.5-4.3%), 52% of whom were newly diagnosed. 17% diabetics had DR giving a prevalence of 0.57%(95%CI 0.26-0.11%). There was no view of the fundus in 8 participants, 5 had cataracts. In the 11,877 other participants, 28 had DR, overall prevalence of DR 0.24%(95%CI 0.20-0.34%); and 16(57.1%) did not know they had diabetes. The types of DR were nonproliferative 73.1%, proliferative 10.8%, and maculopathy 51.4%. 23(62.2%) had sight-threatening PDR/maculopathy needing assessment for treatment. Seven persons had normal vision, 27 had visual impairment (VI) and 3 were blind. 59.3% VI was due to refractive errors.
- CONCLUSIONS. In persons with diabetes, there is possible under-ascertainment of DR due to poor view of fundus due to cataracts. The emergence of diabetes and sight-threatening DR as a condition of public health importance informs the need to have services for detecting and treating DR in Nigeria.
INFORMATION TECHNOLOGY TO CONTROL SCREENING FOR DIABETIC RETINOPATHY
E. Stefánsson1,2,3, E. Ólafsdóttir1,3, A. Guðmundsdóttir1,3, T. Bek3,4, T. Aspelund2,3, Ó. Pálsson3, Ó. Þórisdóttir3,4
1 Landspitali, University Hospital, Reykjavik, Iceland
2 University of Iceland, Reykjavik, Iceland
3 Risk Medical Solutions, Reykjavik, Iceland
4 Aarhus University, Aarhus, Denmark
INTRODUCTION: Annual screening for diabetic eye disease is effective, but may be too frequent and costly for low risk patients.
PURPOSE. The purpose is to use computer based individual risk assessment to make diabetic eye screening programs less expensive and safer.
METHODS.We used epidemiological data to create a mathematical algorithm, which calculates individual risk of sight threatening retinopathy. The individual´s risk level is then used to determine his/her screening interval. The program is available on www.risk.is. The algorithm was tested against the diabetes database in Århus, Denmark (5210 patients, 20 years).
RESULTS. In the diabetes database the algorithm (set at risk margin 4%) suggested an average screening interval of 27 months, with a range of 6 to 60 months. 95 patients progressed to sight threatening retinopathy within the recommended screening interval. At risk margin 2% the respective numbers are 17 months and 32 patients. In comparison, with the standard 12 month screening program 149 patients progressed to sight threatening retinopathy within the recommended screening interval.
Our algorithm, at risk margin 4%, increases safety by 36% while reducing cost of diabetic screening programs by 55% as compared to yearly screening exams. At 2% risk margin increased safety was 79% and cost reduction 30%.
CONCLUSIONS. The use of information technology based on epidemiological data allows individual risk assessment, standardization of risk and an individualized determination of screening intervals. The reduction in screening visits decreases cost of diabetic screening programs by more than 50%compared to programs with yearly screening exams.